Background
STIs are a major global health concern and are among the most common infections worldwide. The World Health Organization (WHO) estimates more than 400 million new cases each year of four common STIs: Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), Treponema pallidum (TP/syphilis), and Trichomonas vaginalis (TV). The ongoing epidemics of HIV and viral hepatitis (HAV, HBV and HCV) pose a danger of dramatic resurgence due to changing prevention modalities and diminished worldwide attention. Additionally, there are alarming increases in AMR in NG and Mycoplasma genitalium (MG). Many of these diseases have insidious presentations that facilitate onward transmission and many are also characterized by local damage that predisposes to co-infections. Although rarely fatal, these diseases result in a substantial burden of disease and can carry a substantial risk of morbidity due to complications such as pelvic inflammatory disease, ectopic pregnancy, infertility, chronic pelvic pain, seronegative arthropathy, and neurological and cardiovascular diseases.
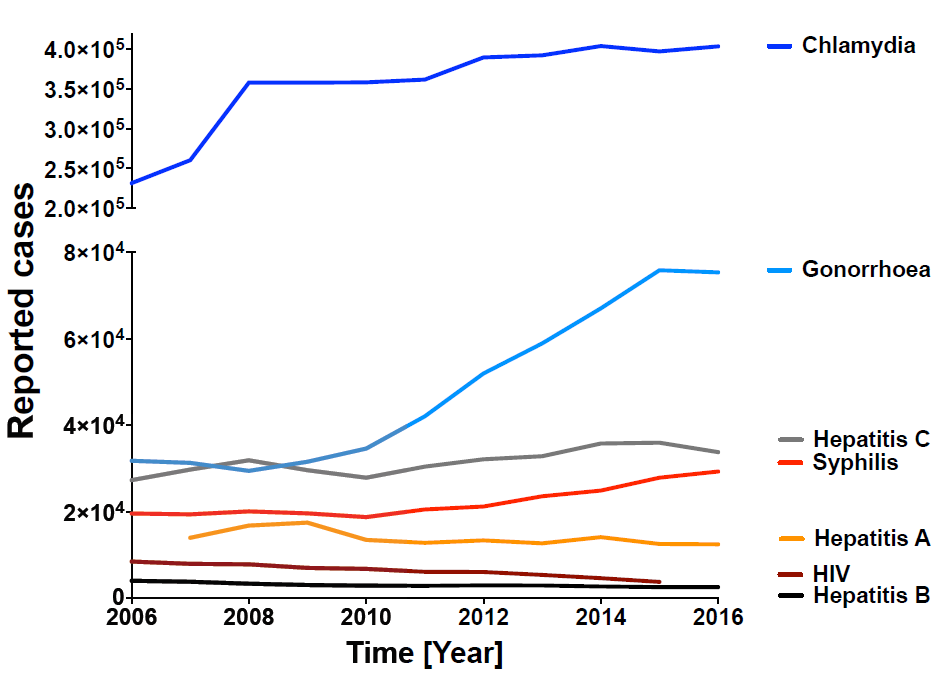
Overall, STIs remain a neglected field for clinical and public health practice and for research. People with STIs experience stigma, STIs disproportionately affect marginalized groups such as sex workers and men who have sex with men (MSM), and condemnatory moral attitudes toward STIs result in unwillingness to prioritize STI control policies. This protocol was developed as a response to the unprecedented rise of STIs in Europe. A factor contributing to this rise was a change in sexual behavioral attitudes due to the newly implemented HIV prevention method, Pre-Exposure Prophylaxis (PrEP). PrEP is an antiviral pill that efficiently protects from HIV infection when taken daily. While PrEP appears to contribute to a significant reduction in new cases of HIV infections, there is evidence that the use of PrEP has led to a reduction in condom use with a resultant increase in other STIs including HCV.
It has been clearly demonstrated that STIs can increase the risk of acquiring HIV infection. Indeed, the spread of HIV and other STIs among MSM has been labeled a syndemic because in this population a number of different and interrelated health problems have come together and interact with one another. The various elements of the syndemic have an additive effect, each one intensifying the others. These factors include the number of infectious diseases endemic in this population, the high rate of substance abuse problems as well as psychological disorders. Recent data from the European Center of Disease Control (ECDC) showed that the proportion of HIV co-infections is highest among MSM with HCV (95–100%) and LGV (35–100%) and is lower for syphilis (20–60%) and gonorrhoea (20–35%). However, methodological limitations and heterogeneity of sources do not allow a comparison across countries and an evaluation of sexual risk behaviors or social background.
To develop and test novel prevention methods or interventions against STIs, knowledge is required on whether there are increased rates of transmission in a given population. In order for trials testing new prevention methods to be cost-effective, the goal is to define a group at risk where there will be at least an annual 3% incidence of new infections of the respective STI. These definitions are based on factors such as gender, age, sexual behavior, economic status and others. However, defining such groups is labor- and cost-intensive and often not do-able for vaccine developers and developers of novel prevention/diagnostic methods. Therefore, only a limited number of novel prevention methods are brought into clinical trials as identification and testing of the most at-risk groups to initially study these products in is too costly. Here we plan to define factors associated with individual STIs or syndemics for potential future prevention trials. Given the increased susceptibility of HIV infection with STI infections, early diagnosis and treatment of STI is substantial to reduce risk factor of HIV acquisition and to inform individuals about their risk of becoming HIV infected. As STIs are a crucial factor in the scope of an incidence analysis of HIV in MSM and are often underdiagnosed, extensive screening measures are implemented within this study.

